What is Colonoscopy?
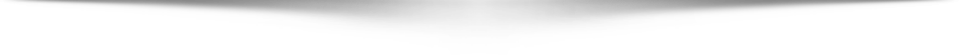
Colonoscopy is an endoscopy test to examine the lining of the whole large bowel (colon). This includes examination of the rectum, sigmoid colon, left/descending colon, transverse colon, right/ascending colon, caecum and terminal ileum (the end of the small bowel). It is more extensive than flexible sigmoidoscopy and is carried out using a thin, flexible tube known as a colonoscope. It is an Outpatient test usually lasting around 20-30 minutes, although cases requiring treatment may take slightly longer. Following the procedure, you may be advised to stay in hospital for up to 2-3 hours after the procedure.
Indications for Colonoscopy
A colonoscopy might be recommended to investigate the following symptoms:
- Anaemia (low blood levels)
- Rectal bleeding
- Abdominal pain
- Change in bowel habit
- To check for causes of diarrhoea
- To check for haemorroids
- To check for diverticular disease
- To check for/ remove polyps
- To check for colorectal cancer
- To check/assess for inflammatory bowel disease (Crohn’s disease, ulcerative colitis)
- To check for defecation disorders (e.g. Post baby delivery)
Alternatives to Colonoscopy
Colonoscopy is a safe, relatively straight forward test and is the gold standard for examining the large bowel. Stool tests such as faecal occult blood tests are useful for screening for bowel cancer and may detect polyps in the general population. If a positive stool test is found then colonoscopy is performed to check for polyps and remove them. Since the introduction of bowel cancer screening and colonoscopy, the number of deaths from bowel cancer has significantly decreased. Virtual CT colonography is a non-invasive scan but it is not as accurate as colonoscopy, can miss the detection of small polyps, does not allow for biopsies to be taken and involves a small dose of radiation. Importantly, once a polyp is found, polypectomy is still needed to remove and treat the polyp which requires colonoscopy. However, there are cases where colonoscopy is not the most suitable test and CT colonography may be more appropriate in these cases.
Preparing for Colonoscopy
Please ensure you tell Dr Goel and the endoscopy team before the day of the procedure if you:
- Are diabetic
- May be pregnant
- Have kidney disease
- Have heart disease
- Have a cardiac pacemaker
- Have a implantable cardiac defbrillator
A strict diet must be followed before the procedure to ensure the bowel is clear of stool and ensure a clear view of the bowel for examination. Drink plenty of fluids, e.g. 2 Litres per day for at least 3 days before the test and avoid eating foods which are high in insoluble fibre (e.g. Bread, nuts, jams, jacket potatoes) for at least 48 hours before the test.
Bowel Preparation
Before the procedure, you will be given a specific bowel preparation medication (e.g. Picolax, Moviprep) and it is very important that you follow the preparation instructions carefully. If performed incorrectly, this may result in a poor quality examination and the test may need to be abandoned or repeated. Do not hesitate to discuss with Dr Goel or the endoscopy nurses if you have any questions.
Fluids allowed: water, lemonade, orange squash, carbonated soft drinks, black tea or coffee (no milk), clear jelly, ice creams and clear soups. Avoid alcohol.
24 hours before the examination
Do not eat any solid foods until after your examination but you can drink plenty of clear fluids. Bowel prep can work rapidly (e.g. Within 15 minutes) or can take up to 3 hours to work. Make sure you are close to a toilet whilst taking bowel prep.
For a morning appointment (08.00-13.00):
- At 14.00 dissolve 1 sachet of bowel prep in 1 pint of lukewarm water and drink over 1 hour
- At 19.00 dissolve 1 sachet (the 2nd) of bowel prep in 1 pint of lukewarm water and drink over 1 hour
For an afternoon appointment (13.00-17.00):
- At 19.00 dissolve 1 sachet of bowel prep in 1 pint of lukewarm water and drink over 1 hour
- At 07.00 (morning of the examination) dissolve 1 sachet (the 2nd) of bowel prep in 1 pint of lukewarm water and drink over 1 hour
Medication Advice
Most usual medications can be continued up till the procedure, however, specific precautions may be taken in some cases. If taking constipating agents such as iron tablets, loperamide (Imodium), codeine phosphate, etc., these should be stopped 1 week prior to examination. Also, if taking any blood-thinning drugs (e.g. Clopidogrel, warfarin, apixaban), it is particularly important to discuss these with Dr Goel or your nurse beforehand so appropriate advice can be given. Please also mention any allergies you may have in advance of your test.
The Colonoscopy Procedure
Upon your arrival, you will be greeted by a member of staff who will help you prepare for your procedure. Your nurse will ask you a few pre-assessment questions and you should inform them of your medications, allergies and any potential concerns. You will also be asked about your arrangements for getting home. You will have a chance to discuss any concerns and ask any questions to ensure you understand the procedure. Dr Goel will discuss the procedure with you and ask you to sign a consent form.
Your nurse will ask you to remove your lower garments and change into a hospital gown in a private changing area. You will have an opportunity to visit the toilet and evacuate your bowels. Once ready, you will be escorted into the procedure room where the endoscopy nurses will introduce themselves and you will have the opportunity to ask any more questions.
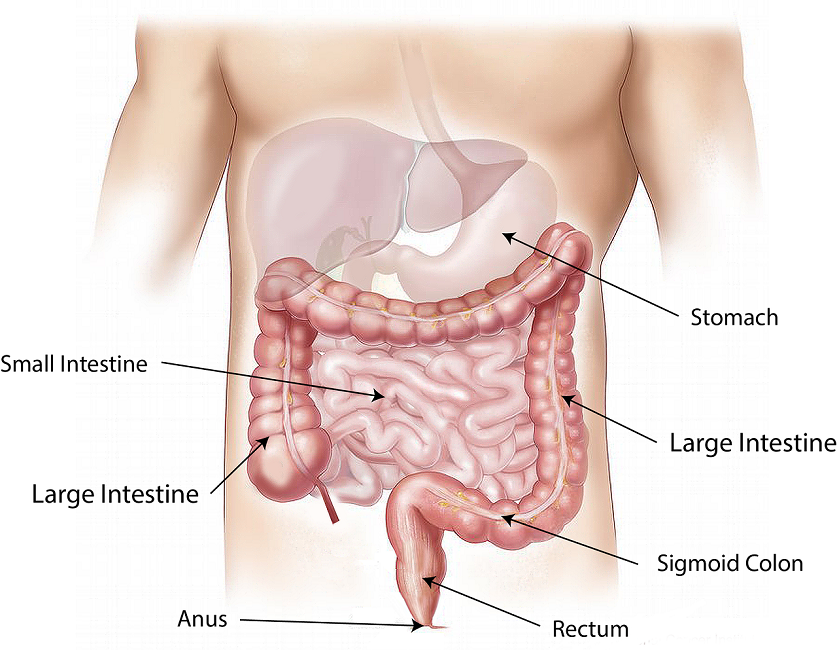
You will be asked to lie on a trolley on your left side. The nurse will monitor your oxygen levels during the procedure with a simple finger probe. A simple rectal examination will be performed which also serves to lubricate the anal passage. The colonoscope will be gently inserted into the rectum (back passage) and the examination usually takes about 20 – 30 minutes to complete. During the procedure, patients may experience bloating and slight discomfort within the abdomen but this usually passes quickly. If needed, additional sedation and painkillers can be given to keep you comfortable. A nurse will be with you at all times to talk to you and also explain what is happening as well as monitoring your oxygen levels and heart rate. Do not feel embarrassed if you need to pass wind as this is quite normal and expected as air is introduced into the bowel during the procedure.
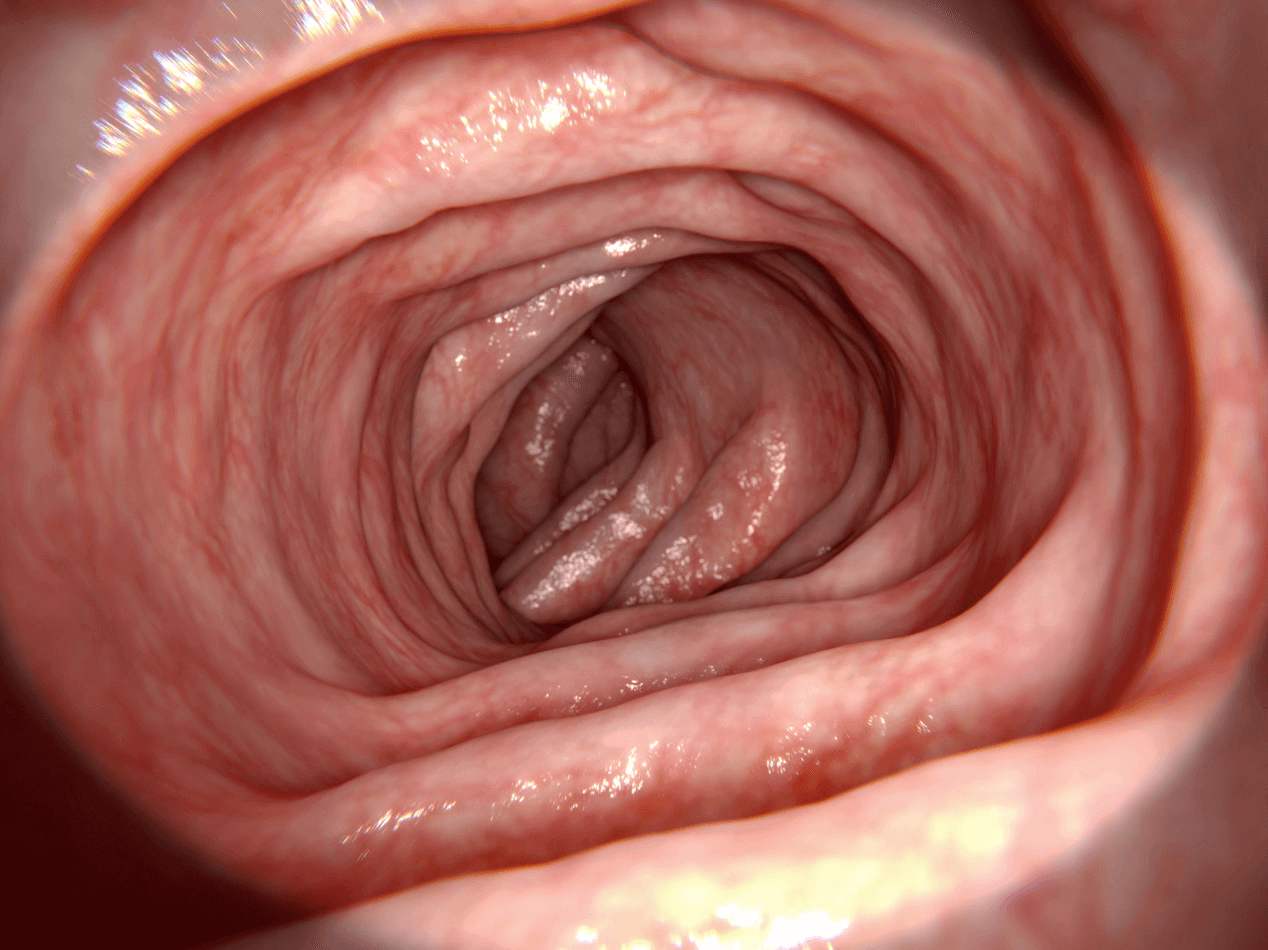
In some cases, a biopsy may be taken from the lining of the bowel which is quite routine and these are sent for analysis. Photos are routinely taken for records and quality assessment. If necessary, small instruments may also be passed through the colonoscope, for example, to remove polyps (usually benign growths). Rarely, the colonoscope cannot be passed through to the end of the large bowel and it may be necessary to withdraw the scope without a full examination. Reasons for this include abnormal narrowing, severe inflammation and poor bowel preparation. Dr Goel will advise you on whether any alternative tests are required.
Sedation and Anaesthesia
As colonoscopy can involve a degree of discomfort, the procedure is usually performed with an intravenous sedative and painkiller. Sedation often makes you drowsy after the procedure and you will require an escort to take you home. You will have the opportunity to discuss sedation and pain relief with Dr Goel before your procedure. Following the procedure, Dr Goel will explain the results of your procedure and answer any questions you may have. It is always advisable to arrange a follow-up appointment to discuss findings (and any awaited biopsy results), particularly if you are tired and drowsy following the procedure as you may not recall what is said. You will be monitored in a recovery bay until the medication has worn off. After sedation, you should avoid driving or operating heavy machinery for 24 hours after the procedure. Sedation is very safe, however, there is a very small risk of over-sedation and with any medication there is a small risk of side-effects.
After the Colonoscopy Procedure
After the procedure, you may feel slightly bloated from air introduced into the bowel during the test, however, this usually passes within a few hours. You will be taken to a recovery area and allowed to rest for as long as necessary whilst observations are made. You can usually eat and drink straight away.
Dr Goel will give you a full written report and explain the findings as well as any treatment or further investigations required. Patients receiving sedation feel very relaxed and sedation can also temporarily affect memory. It is good idea to have an escort (e.g. A family member or friend) with you so the test results can be discussed together. Your escort will be asked to accompany you home when you are ready to leave the department.
If you begin to experience severe pain or experience any bleeding after being discharged, you should see an emergency doctor right away.
Risks of Colonoscopy
Colonoscopy is generally safe and complications are rare. The overall complication rate is approximately 1 in 10000 cases. Possible complications include drug allergies, making a small hole in the bowel (perforation), bleeding and over-sedation. Removal of a polyp (polypectomy) carries a risk of 1 in 500 of causing perforation and a 1 in 100 chance of causing bleeding. If a complication does occur, some cases can be managed at the time of investigation, but surgery may be required. Rarely, abnormalities may be missed which is why it is crucial to follow the bowel preparation instructions and have a thorough endoscopic examination. The test can be more stressful for patients with heart or lung disease and this should be discussed with Dr Goel beforehand. Dr Goel will always ensure any investigation is safe and appropriate for you. Any risks of the procedure will be discussed with you and you will be fully informed beforehand.